Simple Winter Lung Care Tips to Prevent Asthma and Bronchitis
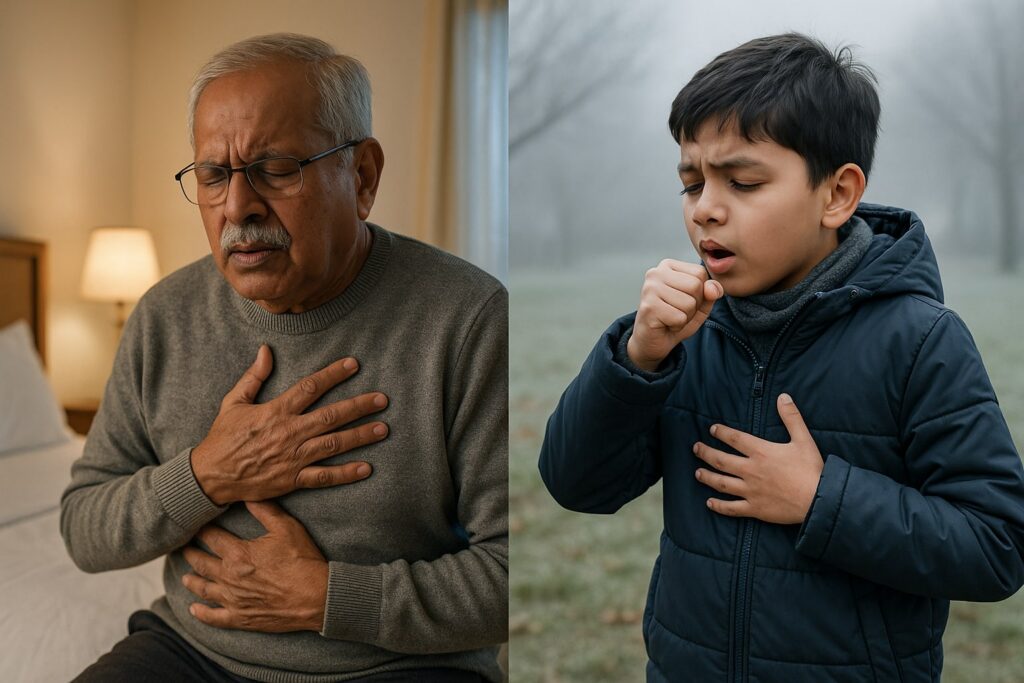
Winter is a challenging period for individuals with asthma, bronchitis, COPD, and other chronic respiratory conditions. The drop in temperature, dry air, increased pollution levels, and higher rate of viral infections contribute to a surge in breathing difficulties during the season. Understanding how winter affects the lungs and adopting preventive measures can significantly reduce flare-ups and improve overall respiratory health.
This article explains why asthma and bronchitis symptoms worsen in winter and outlines practical steps recommended by pulmonologists to maintain lung health.
Why Asthma and Bronchitis Worsen During Winter
During winter, the air becomes colder and drier. When this air reaches the respiratory tract, it irritates and narrows the airways—a reaction known as bronchoconstriction. This leads to increased coughing, wheezing, shortness of breath, and chest tightness.
Several additional factors contribute to worsened respiratory symptoms during winter:
- Higher exposure to indoor allergens due to closed windows
- Increased levels of outdoor pollution and smog
- Seasonal viral infections such as influenza
- Irritants from heaters, incense, and cooking smoke
- Sudden temperature fluctuations between indoor and outdoor environments
Individuals with asthma, chronic bronchitis, or weakened immunity are particularly vulnerable to these triggers.
Symptoms That Require Medical Attention
Winter-related respiratory symptoms can escalate rapidly if not managed appropriately. Seek medical evaluation if you experience:
- Persistent morning chest congestion
- Increased breathlessness during mild physical activity
- Wheezing or noisy breathing
- Tightness or heaviness in the chest
- Frequent night-time coughing
- Higher dependence on rescue inhalers
For specialized evaluation and treatment, you may refer to our Pulmonology Services available here:
Pulmonology Hospital in Faridabad
Evidence-Based Ways to Prevent Asthma and Bronchitis Flare-Ups in Winter
1. Wear a Mask or Scarf Outdoors
Covering the nose and mouth helps warm and humidify the air before it enters the lungs. This reduces airway irritation and prevents bronchospasm triggered by cold air.
2. Maintain Adequate Ventilation Indoors
Keeping windows closed for long periods increases indoor pollutant concentration, dust, and allergens. Ventilate your home during midday hours when pollution levels are relatively lower.
3. Avoid Sudden Temperature Changes
Rapid shifts from warm indoor environments to cold outdoor air can provoke airway narrowing. Use layered clothing, avoid rushing between temperature zones, and allow your body to adjust gradually.
4. Stay Hydrated
Cold air leads to dehydration of the airway lining, causing thicker mucus and breathing difficulty. Adequate hydration thins mucus and helps maintain airway function. Prefer warm water and warm fluids during winter.
5. Use a Humidifier with Proper Maintenance
A balanced indoor humidity level (around 40–50%) prevents airway dryness. However, humidifiers must be cleaned regularly to avoid bacterial or fungal growth, which can worsen respiratory symptoms.
6. Continue Prescribed Inhaler Therapy
Discontinuing or reducing maintenance inhalers during winter is a common cause of exacerbations. Follow your prescribed inhaler routine consistently as directed by your pulmonologist.
7. Reduce Indoor Allergen Exposure
Common winter allergens include dust mites, pet dander, mold, scented products, and smoke. Clean living spaces regularly, use hypoallergenic bedding, and avoid burning incense or mosquito coils.
8. Practice Lung-Strengthening Breathing Exercises
Breathing exercises such as diaphragmatic breathing and pursed-lip breathing help improve lung capacity and reduce breathlessness. Steam inhalation may also provide relief from congestion when recommended by a doctor.
9. Stay Updated with Flu and Pneumonia Vaccinations
Respiratory infections significantly worsen asthma and bronchitis symptoms. Annual flu vaccination and pneumococcal vaccination (as recommended for your age or condition) help reduce complications.
Reference: Centers for Disease Control and Prevention (CDC) – Respiratory Health and Vaccination Guidelines
External link: https://www.cdc.gov/lung-health
10. Seek Early Medical Consultation
Delaying treatment may lead to severe flare-ups, longer recovery time, and increased risk of complications. Early evaluation by a pulmonologist ensures timely intervention, accurate diagnosis, and appropriate treatment.
For comprehensive respiratory care, diagnostic tests such as spirometry, and personalized treatment plans, visit our dedicated pulmonology department.
Daily Winter Lung Care Routine
| Recommendation | Purpose |
|---|---|
| Drink warm water frequently | Maintains airway moisture and reduces mucus thickness |
| Perform light morning exercise | Enhances lung function and circulation |
| Use masks while stepping outdoors | Reduces exposure to cold air and pollutants |
| Maintain clean indoor spaces | Minimizes allergens and respiratory irritants |
| Practice breathing exercises | Supports lung strength and improves airflow |
Conclusion
Winter presents unique challenges for individuals with asthma, bronchitis, and other chronic respiratory conditions. By understanding seasonal triggers and adopting preventive measures, most winter flare-ups can be avoided. Consistent treatment, lifestyle modifications, and timely medical intervention significantly improve outcomes.
If you experience ongoing breathing difficulties or frequent winter exacerbations, consult a pulmonologist for a detailed assessment and personalized management plan.
[…] conditions. Managing respiratory health during this period becomes critical, and following proper winter lung care to prevent asthma and bronchitis can help reduce complications and protect lung […]