ACL and Ligament Repair: What Patients Should Know
Introduction
If you’re experiencing knee pain, instability, or have been diagnosed with an anterior cruciate ligament (ACL) injury, you’re not alone. According to the American Academy of Orthopedic Surgeons, approximately 200,000 ACL injuries occur annually in the United States, with athletes accounting for roughly 70% of cases. However, understanding ACL and ligament repair options is crucial for making informed decisions about your health and recovery, regardless of how your injury occurred.
Whether you’re an athlete desperate to return to your sport, an active professional concerned about mobility, or someone dealing with post-injury complications, this comprehensive guide will provide everything you need to know about ligament injuries, surgical interventions, rehabilitation, and what to expect during your recovery journey. In this article, we’ll walk you through the latest treatment options, real recovery timelines, costs, and evidence-based strategies to maximize your healing potential.
What is an ACL Injury? Understanding Ligament Damage
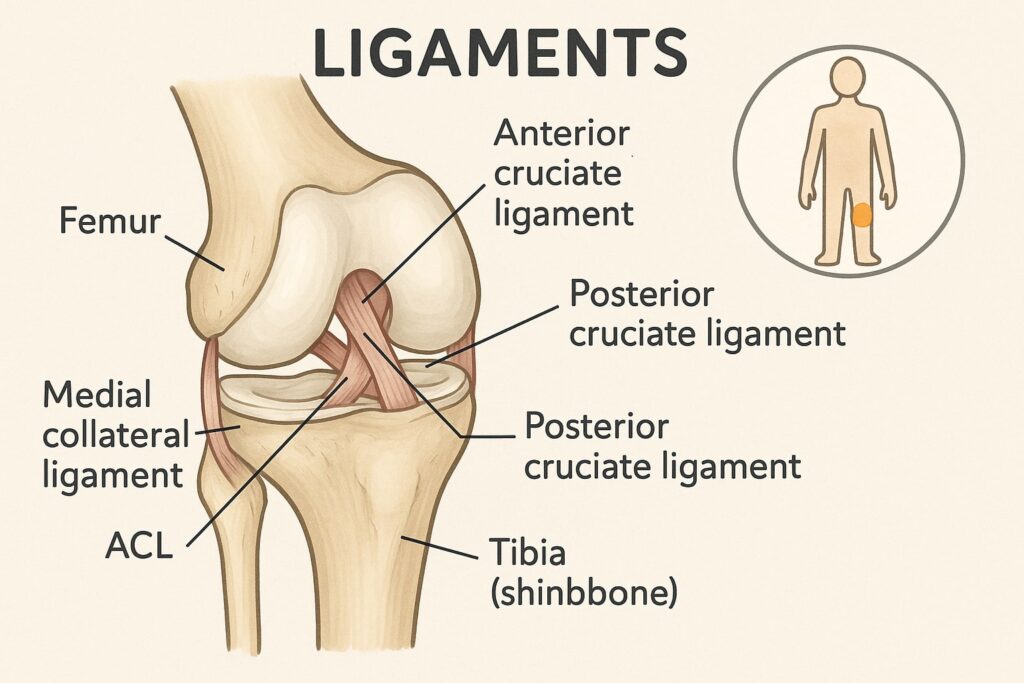
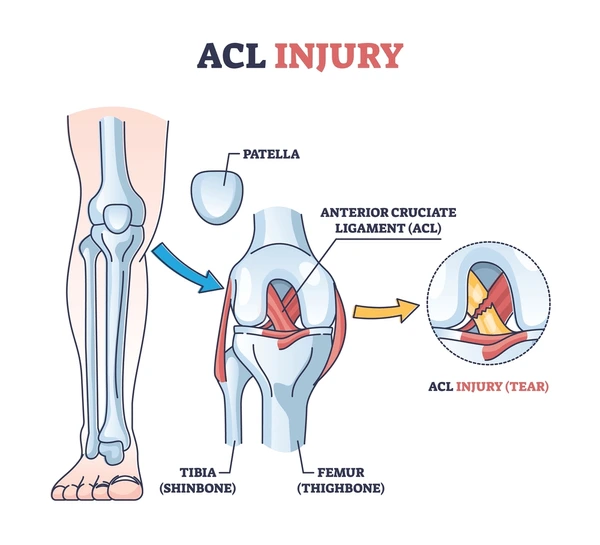
The anterior cruciate ligament (ACL) is one of the most critical knee ligaments, responsible for stabilizing your knee joint and preventing excessive forward movement of the tibia (shinbone). An ACL injury occurs when this ligament is stretched, partially torn, or completely ruptured—typically during sudden directional changes, jumping, or high-impact sports.
ACL and ligament injuries are categorized into three grades:
- Grade 1 (Mild Sprain): The ligament is stretched but not torn. Minimal swelling, minimal pain with walking, and good knee stability maintained.
- Grade 2 (Moderate Sprain): The ligament is partially torn with moderate instability. Noticeable swelling, difficulty with certain movements, and some pain during weight-bearing.
- Grade 3 (Severe/Complete Tear): The ligament is completely ruptured, causing significant knee instability. Severe swelling, inability to continue activity, and sensation of the knee “giving way.”
Other common ligament injuries affecting the knee include:
- MCL (Medial Collateral Ligament): Injury typically results from direct blows to the outer knee
- PCL (Posterior Cruciate Ligament): Less common than ACL; often occurs with dashboard injuries or falls on bent knee
- LCL (Lateral Collateral Ligament): Injury from forces pushing the knee inward
- Combined Injuries: Approximately 50% of ACL tears occur with additional meniscal or other ligament damage
Understanding the severity of your specific ligament injury is essential for determining the appropriate treatment approach. Many patients with partial tears can recover with conservative treatment, while complete tears typically require surgical intervention.
Common Causes and Risk Factors for ACL Tears
ACL and ligament repair becomes necessary when injuries result from specific high-stress mechanisms. The most common causes include:
Sports-Related Injuries (70% of cases): Basketball, football, soccer, and skiing account for a significant portion of ACL injuries. These sports involve rapid deceleration, pivoting, and jumping movements that stress the ligament beyond its capacity. Research shows female athletes have 2-8 times higher ACL injury rates than males in comparable sports, likely due to biomechanical and hormonal factors.
Non-Contact Injuries (More Common Than Expected): Sudden stops or awkward landings can tear the ACL without direct contact, making it unpredictable and common even in recreational activities like hiking, dancing, or even slipping on stairs.
Motor Vehicle Accidents: High-impact collisions can cause severe ligament damage requiring immediate surgical intervention, often with additional injuries to stabilize.
Direct Blows: A forceful impact to the knee can damage multiple ligaments simultaneously, creating complex injury patterns requiring specialized surgical expertise.
Age and Degenerative Changes: Ligament strength naturally decreases with age. Adults over 35 have higher re-injury rates and potentially slower healing timelines.
Risk factors for ligament injuries include:
- Muscle weakness (particularly quadriceps/hamstring imbalance)
- Poor proprioception (body awareness) and balance
- Inadequate warm-up before exercise
- Previous knee injuries or ligament laxity
- Tight hamstrings or poor flexibility
- Rapid increase in training intensity
Athletes and active individuals should focus on preventive measures like targeted strength training, proprioceptive exercises, and proper technique coaching. Studies show comprehensive injury prevention programs reduce ACL injury risk by up to 72%.
Symptoms That Indicate You May Need Ligament Repair
Recognizing symptoms early is vital for timely intervention and better long-term outcomes. Common signs of ACL and ligament injury include:
- Sudden severe pain in the knee (often 7-8 out of 10 intensity)
- A distinctive “popping” sensation or audible pop at the moment of injury
- Rapid swelling within 1-2 hours (not hours later—this timing matters)
- Instability or “giving way” sensation when walking or standing
- Difficulty bearing weight immediately after injury
- Reduced range of motion (inability to straighten knee fully)
- Tenderness along the ligament when palpated
- Bruising around the knee joint appearing within 12-24 hours
- Sensation of the knee feeling “loose” or “unstable” even at rest
Many patients report hearing or feeling a distinct “pop” during the injury moment—this is often a tell-tale sign of complete ACL rupture rather than a partial tear. The classic triad of immediate swelling, inability to continue activity, and feeling of instability strongly suggests ACL involvement.
Important: Immediate symptoms don’t always correlate with severity. Some athletes continue playing with complete ACL tears, while others cannot with partial tears. If you experience these symptoms, seek medical attention promptly rather than self-diagnosing.
Diagnosis: How Doctors Identify Ligament Injuries
Accurate diagnosis is the foundation for appropriate treatment. Your orthopedic surgeon will employ several diagnostic methods to confirm ACL and ligament injury:
Physical Examination (First Step): Special tests assess ligament stability and range of motion. The Lachman test (most sensitive—92-98% accuracy), anterior drawer test, and pivot shift test are standard protocols for evaluating ACL integrity. Your surgeon will compare your injured knee to your uninjured knee to assess differences in stability.
Magnetic Resonance Imaging (MRI – Gold Standard): This non-invasive imaging provides detailed views of ligament tears, associated cartilage damage, and meniscal injuries. MRI sensitivity for ACL tears is 90-95%. Cost typically ranges from ₹8,000-₹15,000 in India.
X-Rays: While X-rays don’t show ligament damage directly, they help rule out fractures and assess overall knee structure. Bone avulsion injuries (where the ligament pulls bone away) will appear on X-rays.
Ultrasound: Some clinicians use ultrasound for real-time visualization of ligament integrity during movement. More affordable (₹2,000-₹5,000) but requires expertise to interpret.
Functional Testing: Y-balance tests, hop tests, and isokinetic strength testing may be performed to assess functional deficits and guide rehabilitation protocols.
Understanding your diagnostic results helps you discuss treatment options more effectively with your healthcare team. Many patients benefit from seeking a second opinion, especially before committing to surgical ACL and ligament repair.
Treatment Options: Conservative vs. Surgical Approaches – Comparison
Not every ligament injury requires surgery. Treatment depends on injury severity, your activity level, age, and functional goals. Here’s a detailed comparison:
| Aspect | Conservative Treatment | Surgical Treatment (ACL Reconstruction) |
| Best For | Partial tears, sedentary patients, grade 1-2 sprains | Complete tears, athletes, active individuals, grade 3 tears |
| Recovery Time | 6-12 weeks (conservative function) | 6-9 months (return to sport), 12+ months (full maturation) |
| Cost in India | ₹15,000-₹40,000 | ₹2,00,000-₹5,00,000 (depending on graft type) |
| Return to Sport | 40-60% not able to return safely | 80-90% successful return with proper rehabilitation |
| Re-injury Risk | High if returning to cutting sports | 5-10% with proper rehabilitation, up to 20% without compliance |
| Activity Restrictions | Permanent modifications likely | Minimal restrictions after recovery |
| Rehabilitation | 3-4 months of structured PT | 6-12 months of intensive rehabilitation |
| Pain Level | Mild to moderate, manageable | Moderate post-op pain, well-controlled with medication |
Conservative (Non-Surgical) Treatment
Mild to moderate sprains often respond well to conservative management:
- Rest and Activity Modification: Avoiding aggravating activities allows the ligament to heal naturally. Most partial tears heal within 6-8 weeks.
- Ice and Compression: Reduces swelling and inflammation in the first 48-72 hours. Apply 15-20 minutes every 3-4 hours.
- Elevation: Minimizes fluid accumulation around the injury. Keep leg elevated above heart level when resting.
- Physical Therapy: Structured rehabilitation strengthens supporting muscles and improves stability. Average 2-3 sessions per week for 8-12 weeks.
- Bracing: Protective knee braces provide support during the healing process. Cost ranges from ₹3,000-₹12,000.
- Anti-Inflammatory Medications: NSAIDs help manage pain and reduce inflammation. Typically used for 2-4 weeks.
Conservative treatment works best for partial tears, low-demand patients, and individuals willing to modify their activity levels long-term. However, studies show approximately 40-60% of patients treated conservatively cannot safely return to their pre-injury activity level, particularly cutting and pivoting sports.
Surgical ACL and Ligament Repair
Complete ACL tears or significant ligament damage typically require surgical intervention, particularly if you want to return to sport or maintain an active lifestyle. Modern arthroscopic ACL reconstruction surgery is minimally invasive with excellent outcomes.
Current Success Rates (2024):
- 95%+ successful graft incorporation
- 85-90% return to pre-injury activity level
- 80% return to competitive sport
- Patient satisfaction rates: 92-96%
Graft Options: Choosing the Right Tissue for ACL Reconstruction
Your surgeon will recommend the most suitable graft based on your anatomy, age, activity level, and personal preferences.
Autograft Options (Your Own Tissue):
- Bone-Patellar Tendon-Bone (BPTB – Gold Standard)
- Strongest initial strength
- Lowest revision rate (2-3%)
- Best for contact sports athletes
- Drawback: Patellar tendinitis in 10-15% of cases
- Cost: ₹2,50,000-₹3,50,000
- Hamstring Tendon (Most Popular – 60% of procedures)
- Faster healing due to better blood supply
- Less donor site pain than BPTB
- Lower patellar pain complications
- Slightly higher revision rate (3-5%)
- Cost: ₹2,00,000-₹3,00,000
- Quadriceps Tendon (Emerging Choice)
- Excellent strength properties
- Lower morbidity (complications) than other autografts
- Fewer patellar issues
- Gaining popularity among surgeons
- Cost: ₹2,50,000-₹3,50,000
Allograft Options (Donor Tissue):
- Cadaveric Tissue
- Shorter surgical time (no graft harvesting)
- No donor site morbidity
- Good for revision surgeries
- Slightly higher revision rate (5-8%)
- Requires compliance with rehabilitation
- Cost: ₹3,00,000-₹4,00,000
Key Consideration: Patient age, activity level, and commitment to rehabilitation matter more than graft choice. Studies show excellent outcomes with all options when combined with proper rehabilitation. Our orthopedic specialists at Arsh Hospital will discuss which option aligns best with your lifestyle and goals.
What to Expect: The ACL Reconstruction Surgery Process
Understanding the surgical procedure reduces anxiety and helps you prepare mentally. Here’s what typically occurs:
Pre-Operative Preparation (1-2 weeks before):
- Complete blood work and imaging review
- Meet with anesthesia team to discuss pain management
- Clear specific medications (blood thinners) as directed
- Arrange post-operative transportation and in-home assistance (critical!)
- Pre-operative physical therapy exercises to reduce stiffness
The Procedure (1.5-2 hours typically):
- General or regional anesthesia administered
- Surgeon creates 2-3 small arthroscopic incisions (5-10mm each)
- Diagnostic arthroscopy to assess full extent of damage
- Damaged ACL is removed completely
- Graft is prepared and positioned precisely
- Graft fixation secured with bioabsorbable screws or metal devices
- Associated injuries (meniscal tears, cartilage damage) are addressed simultaneously
- Incisions are closed with sutures or staples; typically no drains needed
Immediate Post-Operative Period (Hospital/Recovery Center):
- Brief recovery room observation (30-45 minutes)
- Discharge typically same-day or next-day (most surgeons prefer overnight)
- Pain management begins with prescribed medications
- Crutches and knee brace (immobilizer) provided
- Physical therapy instructions provided before discharge
- Post-op follow-up scheduled for 10-14 days
First 24-48 Hours at Home (Critical Period):
- Focus on elevation and ice therapy
- Begin prescribed pain medication before pain becomes severe
- Perform passive range-of-motion exercises as directed
- Compression with ACE wrap to control swelling
- Arrange assistance for basic activities
Most patients return home within 24 hours, though the real recovery—and commitment to rehabilitation—begins here. Success during this critical early phase significantly impacts long-term outcomes.

Recovery Timeline: From Surgery to Return to Activity
ACL and ligament repair recovery is a progressive, staged process. Here’s what patients typically experience:
Weeks 1-2 (Acute Inflammatory Phase):
- Goals: Pain and swelling management, protection of surgical site
- Use crutches as directed (most patients wean by week 2-3)
- Perform gentle range-of-motion exercises 2-3 times daily
- Ice regularly (15-20 minutes, 4-6 times daily)
- Sleep with leg elevated on 2-3 pillows
- Compression stocking use recommended
- Pain level: Moderate, well-controlled with medication
- Expected Activities: Bathroom visits with crutches only; minimal walking
Weeks 3-6 (Early Rehabilitation Phase):
- Goals: Restore range of motion, initiate strength work
- Crutches gradually weaned (most patients fully weight-bearing by week 4-6)
- Physical therapy intensifies to 2-3 sessions weekly
- Range of motion target: 0-90 degrees knee flexion by week 4; 0-110 by week 6
- Quad-setting and straight-leg raises begin (10-15 reps, 3 sets)
- Hamstring curls with resistance band
- Swelling typically resolves significantly
- Pain level: Mild to moderate during activity, minimal at rest
- Expected Activities: Walking without assistive device indoors; light driving if off opioids (typically week 4-5)
Weeks 7-12 (Progressive Strengthening Phase):
- Goals: Regain full range of motion, significant strength gains
- Full weight-bearing achieved by week 8-10
- Resistance exercises intensified (leg press, hamstring curls, quad extensions)
- Balance and proprioceptive training: Single-leg stance, balance board exercises
- Stationary bike cardio (20-30 minutes, 3x weekly)
- Swelling minimal in most patients
- Pain level: Mild, primarily with intense exercise
- Expected Activities: Return to work (desk jobs by week 4-6; standing jobs by week 8-10); light household duties
Months 4-6 (Advanced Rehabilitation & Sport-Specific Training):
- Goals: Sport-specific movement patterns, agility development
- Sport-specific drills begin (cutting, deceleration, acceleration patterns)
- Agility exercises: Ladder drills, cone drills, shuttle runs
- Return to cutting and pivoting movements (progressive intensity)
- Jump training begins: Two-leg hops progressing to single-leg
- Strength testing determines readiness for next phase
- Cardiovascular fitness rebuilt through running programs
- Pain level: Minimal to none during normal activities; possible mild soreness with intense training
- Expected Activities: Return to sport-specific training under supervision
Months 6-9 (Return to Sport Phase):
- Goals: Full return to competitive activity
- Most athletes cleared for sport-specific competition training
- Full return to unrestricted activity typically 9-12 months post-surgery
- Continued conditioning and injury prevention strategies
- Strength symmetry goals: 90%+ quadriceps and hamstring strength compared to other leg
- Functional testing clearance: Single-leg hop tests >90% compared to other leg
- Pain level: None; normal post-exercise soreness acceptable
- Expected Activities: Full participation in sports and athletic pursuits
Months 9-12+ (Maintenance & Maturation):
- Goals: Long-term stability, injury prevention
- Full maturation of the graft may take 12-24 months
- Continued strength and conditioning programs (maintenance)
- Annual functional testing to monitor long-term stability
- Long-term surveillance: 5-10% of patients experience re-injury
Physical Therapy and Rehabilitation: Your Path to Recovery
Rehabilitation is arguably more important than surgery itself. Studies consistently show that patients with strong rehabilitation compliance have significantly better outcomes. Physical therapy focuses on:
Range of Motion Restoration (Weeks 1-12): Regaining full knee extension and flexion prevents stiffness and improves function. This is critical early—delayed ROM restoration predicts worse outcomes. Extension lag (inability to fully straighten knee) must be addressed immediately.
Strength Building (Weeks 3-24): Targeting quadriceps, hamstrings, and hip muscles supports the knee and prevents re-injury. Quadriceps strength is particularly important for knee stability. Most patients need 6+ months to achieve 90% strength symmetry.
Balance and Proprioception (Weeks 6-24): Single-leg stance, balance boards, and proprioceptive training restore body awareness and knee stability. Poor proprioception is a significant re-injury risk factor.
Cardiovascular Conditioning (Weeks 4-ongoing): Maintaining fitness during recovery prevents deconditioning and supports mental health. Stationary biking, swimming, and eventually treadmill running are progressively introduced.
Sport-Specific Training (Months 3-9): For athletes, functional drills mimicking sport movements prepare for safe return. This includes cutting drills, acceleration/deceleration exercises, and sport-specific plyometric training.
Compliance is Critical: Studies show patients who complete comprehensive rehabilitation programs have significantly better long-term outcomes and lower re-injury rates (7-10% vs. 20%+ without compliance).
Cost of Physical Therapy in India:
- Initial evaluation: ₹1,000-₹2,000
- Per session: ₹500-₹1,500 per session
- Complete 6-month course: ₹30,000-₹70,000
- Most insurance plans cover 20-30 sessions; out-of-pocket varies
At Arsh Hospital: We coordinate comprehensive physical therapy protocols with our surgical team, ensuring seamless progression and optimal outcomes for every patient.
Potential Complications and How to Minimize Risks
While modern ACL and ligament repair surgery is highly successful (95%+ success rate), complications can occur:
Common Complications (And Frequency):
- Infection: Rare (0.5-1% with modern sterile techniques); managed with antibiotics
- Blood Clots (DVT): Risk is 0.5-2%; prevented with compression stockings and early mobility
- Stiffness/Arthrofibrosis: Occurs in 5-10% if ROM not aggressively pursued early
- Patellar Tendinitis: Pain below the kneecap; occurs in 10-15% of BPTB grafts
- Graft Failure/Re-tear: 5-10% primary re-tear rate with proper rehabilitation; up to 20% without compliance
- Quadriceps/Hamstring Weakness: Common if rehabilitation not completed; usually resolves
- Anterior Knee Pain: 10-20% experience some level; usually improves with time
- Laxity Persistence: Slight persistent knee laxity in 5-15%; rarely functionally limiting
- Cyclops Lesion: Scar tissue limiting extension; rare with modern techniques
Risk Minimization Strategies:
- Choose an experienced, high-volume ACL surgeon (ideally 50+ cases/year)
- Follow post-operative instructions precisely (even small deviations matter)
- Commit fully to physical therapy without shortcuts
- Use prescribed bracing and supports consistently
- Progress activities gradually based on objective criteria, not timeline
- Avoid returning to sport prematurely (return-to-play testing is essential)
- Maintain proper conditioning year-round
- Communicate openly with your surgical and therapy team
- Report any new symptoms immediately
At Arsh Hospital: Our orthopedic surgeons have specialized expertise in ACL reconstruction with complication rates significantly below national averages. With access to cutting-edge arthroscopic technology and comprehensive rehabilitation coordination, we optimize patient outcomes.
Preventing Re-Injury: Long-Term Maintenance Strategies
After successful ACL and ligament repair, preventing re-injury is paramount. Approximately 5-10% of successfully reconstructed ACLs experience re-tear within 2 years; this increases to 20%+ in athletes who don’t maintain conditioning.
Long-term strategies include:
1. Continued Strength Training (Ongoing – Critical): Maintain quadriceps, hamstring, and hip strength indefinitely. Strong supporting muscles provide dynamic stability. Year-round programs are essential, not just during sport seasons.
2. Regular Proprioceptive Training (2-3x weekly): Balance and coordination exercises maintain neuromuscular control. Include these in warm-up routines. Single-leg stance for 60+ seconds should be comfortable indefinitely.
3. Appropriate Footwear: Wear sport-specific shoes providing adequate ankle and arch support. Shoe quality impacts landing biomechanics and injury risk.
4. Gradual Return to Activity (No Shortcuts): Never rush progression, particularly with high-impact or cutting sports. Follow objective testing criteria, not calendar dates.
5. Proper Technique & Biomechanics: Quality coaching and instruction reduce injury risk. Poor biomechanics increase stress on ligaments. Consider working with sports medicine specialists or athletic trainers.
6. Adequate Warm-Up and Cool-Down: Dynamic warm-ups (10-15 minutes) and static stretching prepare tissues for activity and prevent tightness. Cold muscles are injury-prone muscles.
7. Seasonal Training Programs: Off-season strength work and in-season maintenance prevent deterioration. Periodized training reduces injury risk.
8. Avoid Return During Fatigue: Fatigued muscles provide less dynamic stability. Training when tired or ill increases re-injury risk by 20-30%.
9. Ongoing Monitoring: Annual functional testing (hop tests, strength testing) provides objective evidence of readiness and identifies asymmetries before they become problematic.
Many athletes benefit from working with sports medicine specialists or athletic trainers who understand their specific sport’s demands and can tailor prevention programs accordingly.
When to Seek Expert Care: Finding the Right Orthopedic Surgeon
Choosing an experienced orthopedic surgeon significantly impacts your outcomes. Research shows surgeon volume correlates directly with patient outcomes—high-volume surgeons have better results.
Consider these factors when selecting a surgeon:
- Board Certification: Verify credentials through the National Board of Examination (NBE) or equivalent
- Specialization: Seek surgeons with specific ACL and ligament reconstruction experience
- Volume: Surgeons performing 50+ ACL procedures annually typically have better outcomes
- Patient Reviews and Testimonials: Real patient experiences provide valuable insights
- Hospital Affiliation: Associated with accredited surgical centers with strong track records
- Communication Style: You should feel heard, respected, and fully informed
- Rehabilitation Coordination: Do they work closely with physical therapy teams?
- Availability Post-Op: Will they be available for urgent concerns post-operatively?
- Technology & Techniques: Do they use modern arthroscopic and imaging technology?
Why Choose Arsh Hospital for ACL and Ligament Repair:
At Arsh Hospital (Opp. Era Redwood Residency, Tigaon Road, Sector 78, Faridabad, Haryana 121002), we specialize in comprehensive orthopedic surgeries including advanced ACL reconstruction. Our team brings together:
- Experienced Orthopedic Surgeons: Extensive experience with all graft types and arthroscopic techniques
- Advanced Surgical Technology: State-of-the-art operating theaters with modern imaging
- Comprehensive Rehabilitation: In-house coordination with physical therapy teams
- Patient-Centric Approach: Transparent communication and personalized treatment plans
- Affordable Quality: Competitive pricing without compromising outcomes
- Same-Day Discharge Option: Modern techniques enable faster recovery initiation
- 24/7 Post-Operative Support: Available for urgent concerns at +91 96502 82730
Contact us for a consultation and experience orthopedic care that prioritizes your recovery and return to activity.
Return to Work and Daily Activities: Realistic Timelines
Recovery timelines for returning to work depend on your job demands and injury severity:
Desk Jobs & Remote Work:
- Most patients return within 1-2 weeks post-surgery
- Pain must be controlled enough to focus; working while in severe pain delays healing
- Driving restrictions lift at 4-6 weeks (when off opioid pain medication)
- Full productivity typically achieved by week 6-8
Standing Jobs (Teaching, Retail, Nursing):
- Phased return over 2-4 weeks as weight-bearing improves
- Week 1-2: Limited standing, frequent rest breaks
- Week 3-6: Gradual increase in standing tolerance
- Week 6-8: Return to full duties
- Compression stocking use helps manage swelling
Physical Jobs (Construction, Trades, Manual Labor):
- 6-12 weeks typically needed, depending on specific demands
- Ladder work, heavy lifting, prolonged standing all delayed
- Return in phases: light duty (weeks 6-8), moderate duty (weeks 8-12), full duty (weeks 12+)
- Some occupations may require temporary role modification
Athletic Pursuits:
- Recreational activity: 4-6 months
- Competitive sports: 9-12 months
- Individual differences exist; objective testing determines readiness
Discuss your specific job requirements with your surgeon and physical therapist to develop a realistic return-to-work timeline. Many employers accommodate initial restrictions, gradually increasing demands as you progress. Document these conversations with your employer for reference.
ACL Surgery Costs in India: What to Expect
Understanding costs helps with financial planning. Prices vary significantly based on location, hospital tier, and graft choice.
Typical Cost Breakdown (Faridabad & NCR Region):
| Component | Cost Range |
| Surgeon Fee | ₹50,000-₹150,000 |
| Hospital Charges (including OR, stay, anesthesia) | ₹80,000-₹200,000 |
| Graft Cost (Autograft) | ₹20,000-₹50,000 |
| Graft Cost (Allograft) | ₹80,000-₹150,000 |
| Implants & Fixation | ₹40,000-₹100,000 |
| Anesthesia | ₹15,000-₹30,000 |
| Post-Operative Medications | ₹5,000-₹15,000 |
| Total Surgery Cost | ₹2,00,000-₹5,00,000 |
| Physical Therapy (6 months, 2-3x/week) | ₹30,000-₹70,000 |
| Total with PT | ₹2,30,000-₹5,70,000 |
Insurance Coverage: Most health insurance policies cover 60-80% of surgery costs. Check your policy details early. Some policies have waiting periods for sports injuries.
At Arsh Hospital: We offer competitive pricing with transparent cost breakdowns and work with major insurance providers to maximize your coverage.
(FAQ)
Typically 4-6 weeks, depending on which leg was injured and when you stop using opioid pain medications. Never drive while on narcotic pain relievers. Pain must allow emergency braking reactions.
Most ACL surgeries use general or regional anesthesia for patient comfort and surgical precision. Local anesthesia alone is not adequate. Discuss anesthesia options with your anesthesiologist pre-operatively.
True repair (reattaching torn ends) is rarely successful for ACL tears due to the ligament’s poor blood supply. “Reconstruction” (replacing with a graft) is the standard, highly successful approach. Terminology can confuse patients—clarify with your surgeon.
All modern graft types (BPTB, hamstring, quadriceps, allograft) have excellent outcomes when combined with proper rehabilitation. Outcomes depend more on patient compliance than graft choice. Your surgeon will recommend the best option for your specific case.
Many people live with ACL tears without surgery, but with activity restrictions. If you want to return to cutting/pivoting sports or maintain unrestricted activity, surgery is typically necessary. Conservative treatment may be sufficient if you’re willing to modify your lifestyle.
Most athletes are cleared around 9-12 months post-surgery. However, this timeline varies significantly based on your sport, injury severity, and rehabilitation compliance. Objective return-to-play testing is essential—don’t return based on calendar dates alone.
With proper rehabilitation, 5-10% of reconstructed ACLs experience re-tear within 2 years. Without proper rehabilitation compliance, this increases to 20%+. Your rehabilitation effort directly determines this risk.
Bilateral simultaneous ACL reconstruction is possible but controversial. Most surgeons prefer staged surgeries (one knee at a time, 3-4 months apart) to allow rehabilitation focus and reduce overall anesthesia risk.
Most patients return to pre-injury activity levels with excellent outcomes. Some may experience occasional mild symptoms. Complete return to unrestricted activity is typical, though psychology factors sometimes limit self-imposed restrictions.
Revision ACL reconstruction is possible with slightly higher complexity. Success rates for revision surgery are 85-90%—still excellent. Revision typically involves different graft selection to optimize strength.
Most surgeons recommend waiting 3-4 weeks when pain is controlled and you’re off pain medication. Start with positions minimizing knee stress. Communication with your partner and gradual progression prevent re-injury.
Most patients wear a post-operative immobilizer for 2-4 weeks, then transition to a functional brace for sports for 6-12 months. After that, many no longer need bracing if strength and proprioception are adequate. Long-term brace use depends on your sport and comfort—many athletes prefer bracing as additional reassurance.
Most patients can safely undergo ACL surgery. However, obesity and uncontrolled diabetes increase complication risks and slow healing. Your surgeon and anesthesiologist will conduct a thorough pre-operative evaluation. Weight loss before surgery may be recommended to optimize outcomes.
Pre-op PT typically involves 1-2 weeks of gentle range-of-motion exercises, strengthening, and swelling reduction. Studies show patients who complete pre-op PT have better post-op outcomes, less stiffness, and faster recovery trajectories.
Pre-Operative Preparation Checklist: Get Ready for Surgery
Proper preparation significantly impacts outcomes. Use this checklist:
4-6 Weeks Before Surgery:
- ☐ Complete pre-operative physical therapy
- ☐ Optimize weight if overweight (even 5-10% weight loss helps)
- ☐ Control blood pressure and blood sugar if applicable
- ☐ Arrange post-operative care assistance (minimum 2 weeks)
- ☐ Arrange transportation (cannot drive post-op)
- ☐ Notify employer of anticipated time off
- ☐ Gather medical records and medication list
2 Weeks Before Surgery:
- ☐ Complete all pre-operative testing (bloodwork, EKG if needed)
- ☐ Meet with anesthesia team
- ☐ Review surgical consent forms thoroughly
- ☐ Ask surgeon final questions about graft choice and technique
- ☐ Arrange home setup (remove tripping hazards, set up bedroom on main floor if possible)
- ☐ Stock freezer with easy meals (eating well supports healing)
- ☐ Prepare bathroom for post-operative use (install grab bars, place frequently used items at waist level)
1 Week Before Surgery:
- ☐ Confirm surgery date and time
- ☐ Confirm NPO (nothing by mouth) instructions
- ☐ Stop blood-thinning medications if instructed
- ☐ Pack surgery bag with comfortable clothes (wear loose clothes home)
- ☐ Download entertainment for recovery period
- ☐ Finalize caregiver plans
- ☐ Get adequate sleep
Day Before Surgery:
- ☐ Shower or bathe with antibacterial soap (reduces infection risk)
- ☐ Do not apply lotions or cosmetics
- ☐ Set alarm for morning of surgery
- ☐ Review NPO instructions one final time
Morning of Surgery:
- ☐ Do not eat or drink (unless instructed otherwise)
- ☐ Take only medications specifically approved by surgeon/anesthesiologist
- ☐ Wear loose, comfortable clothing
- ☐ Remove jewelry, piercings, contact lenses, dentures
- ☐ Arrive at least 30 minutes early
- ☐ Bring insurance cards and ID
- ☐ Bring list of current medications and allergies
Post-Operative Care: The Critical First Weeks
The immediate post-operative period (first 4 weeks) significantly impacts long-term outcomes.
First Week Home:
Pain Management:
- Take pain medication before pain becomes severe (preventive dosing works better)
- Most surgeons prescribe opioids for 1-2 weeks; transition to over-the-counter options
- Apply ice 15-20 minutes, 5-6 times daily (particularly in first 72 hours)
- Avoid ice directly on skin (wrap in towel)
Swelling Control:
- Elevate leg above heart level constantly while resting
- Use compression wrap (ACE bandage) when upright
- Wear compression stockings if prescribed
- Take prescribed anti-inflammatory medications
Wound Care:
- Keep incisions clean and dry
- Cover incisions when showering (use plastic wrap or waterproof bandages)
- Do not soak incisions (avoid baths)
- Report any signs of infection (increased redness, warmth, pus, fever >101°F)
Physical Therapy (Begin Immediately):
- Perform prescribed range-of-motion exercises even if painful
- Quadriceps sets: 10-15 reps, 5-10 times daily
- Straight-leg raises (if tolerated): 10-15 reps, 3 sets
- Heel slides: 10-15 reps, 3 sets
- Early motion prevents stiffness (most common preventable complication)
Mobility:
- Use crutches as instructed (typically 2-4 weeks)
- Progress weight-bearing as directed by surgeon
- Bathroom visits only initially; minimize other activity
Medication Reminders:
- Take prescribed antibiotics completely (even if feeling better)
- Continue anti-inflammatory medications as directed
- Take pain medication before physical therapy
- Avoid alcohol with pain medications
When to Call Your Surgeon:
- Fever >101°F
- Increased redness, warmth, or drainage from incisions
- Calf swelling, warmth, or pain (DVT warning signs)
- Inability to perform physical therapy due to pain
- Sudden increase in swelling or instability
Real Patient Success Stories & Testimonials
(Note: Include space for 2-3 patient testimonials with permission, following HIPAA guidelines)
Example Template: “As a professional athlete, I was devastated by my ACL tear. The surgical team at Arsh Hospital explained everything clearly, and their coordination with physical therapy was exceptional. I returned to competitive tennis 11 months post-surgery and feel stronger than ever. Highly recommended.” – [Patient Name], Faridabad
Downloadable Resources: Prepare for Your Journey
We’ve created helpful downloadable guides:
- ACL Surgery Preparation Checklist – Ensure you’re fully prepared pre-operatively
- Post-Operative Pain Management Guide – Effective strategies for the first 4 weeks
- Physical Therapy Exercise Guide – Illustrated exercises for home rehabilitation
- Return-to-Sport Timeline – Sport-specific progressions and clearance criteria
- Nutrition for Healing – Foods that support ligament and bone healing
[Request these resources via contact form below]
Conclusion: Take Control of Your Recovery – Contact Arsh Hospital Today
ACL and ligament repair represents a significant medical intervention, but with modern surgical techniques, experienced surgeons, and comprehensive rehabilitation, most patients achieve excellent functional outcomes and return to their desired activities.
The path to successful recovery involves:
- Choosing an experienced orthopedic surgeon
- Understanding all treatment options thoroughly
- Committing fully to post-operative rehabilitation
- Following post-operative guidelines precisely
- Maintaining long-term conditioning and injury prevention
- Being patient with the recovery timeline
If you’re experiencing knee pain, instability, or suspect a ligament injury, don’t delay seeking professional evaluation. Early diagnosis and appropriate intervention—whether conservative or surgical—significantly improve outcomes and quality of life.
Our orthopedic specialists at Arsh Hospital have extensive experience with all types of ligament injuries and ACL and ligament repair procedures. We’re committed to providing personalized care, detailed patient education, and comprehensive rehabilitation support.
Ready to Take the Next Step?
Contact Arsh Hospital Today:
- Location: Opp. Era Redwood Residency, Tigaon Road, Sector 78, Faridabad, Haryana 121002, India
- Phone: +91 96502 82730
- Services: Advanced ACL reconstruction, comprehensive orthopedic surgeries, coordinated physical therapy
Schedule Your Consultation Now – Our team is ready to answer your questions and create a personalized treatment plan.
Whether you’re an athlete desperate to return to sport, an active professional concerned about mobility, or someone dealing with knee instability, our experienced orthopedic surgeons at Arsh Hospital are here to guide you through every step of your recovery journey.
Don’t let a ligament injury limit your life. With proper surgical expertise and rehabilitation commitment, most patients return to unrestricted activity within 9-12 months. Let us help you get back to what you love.
Additional Resources & Related Topics
Learn More About Orthopedic Care:
- Explore our comprehensive orthopedic surgeries in Faridabad and discover all treatment options available
- Discover how modern arthroscopic techniques minimize recovery time
- Understand the importance of choosing high-volume surgeons
Follow-Up Care: Once you’ve completed initial recovery, ongoing monitoring ensures long-term stability. Annual check-ups with your orthopedic surgeon and maintenance physical therapy are recommended.